Treatment failures are no longer rare occurrences in Nigerian hospitals. Pneumonia, which once responded to first-line antibiotics, now requires stronger, more expensive alternatives. Surgical infections resist multiple drugs. Neonatal sepsis has taken over lives because available antibiotics no longer work. The Nigerian Center for Disease Control and Prevention is tracking these patterns. Documenting rising resistance across pathogens and regions. Because prevention isn’t a distant possibility or theoretical exercise, and can’t be cured by isolating yourself. It’s an urgent necessity demanding immediate, coordinated action from healthcare systems, regulatory bodies, prescribers, and patients themselves.
What Actually Causes Resistance?
The real causes of antimicrobial resistance stem from both biological and behavioral sources. Biologically, bacteria naturally mutate and evolve. But when it is exposed to antimicrobials, susceptible bacteria die while resistant mutants survive and reproduce. This natural selection accelerates with frequent, inappropriate antimicrobial exposure. Behaviorally, humans drive resistance through misuse patterns.
Prescribers give antimicrobials for viral infections that don’t require them. Patients demand antibiotics for conditions that will resolve naturally.
Self-medication allows people to take the wrong drugs, without being aware of the dosage and duration. Agricultural practices contribute too. Farmers use antimicrobials in livestock for growth promotion rather than disease treatment.
These drugs enter food chains and environments, exposing more bacteria to selection pressure. System gaps permit antimicrobials to be sold without prescriptions. Weak regulation fails to control substandard medicines. Each factor compounds the others, creating conditions where resistance thrives.
Prevention of Antimicrobial Resistance
Antimicrobial resistance demands coordinated actions across multiple fronts. It starts with reducing unnecessary antimicrobial use. Prescribers must commit to evidence-based guidelines, ordering antimicrobials only when clinically indicated.
Diagnostic testing should guide therapy rather than empirical guessing. When antimicrobials are necessary, selecting the narrowest spectrum drug that treats the infection effectively limits broader resistance development.
Patients must complete prescribed courses even after feeling better. Stopping early leaves surviving bacteria that develop resistance.
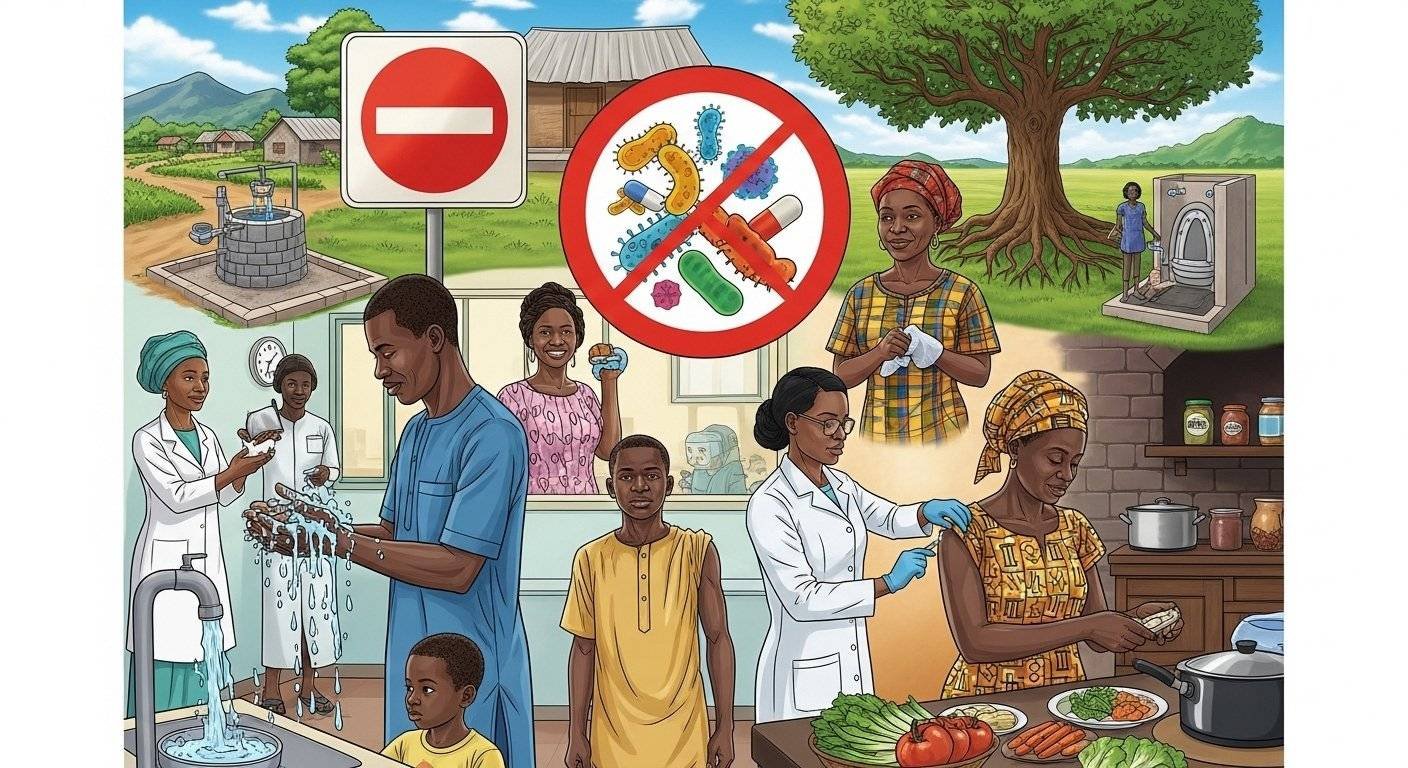
Infection prevention reduces the need for antimicrobials entirely.
- Hand hygiene
- Safe water
- Proper sanitation
- Vaccination programs
- Surgical sterility decreases infection rates
Fewer infections mean fewer antimicrobial exposures and slower resistance development. Surveillance systems must track resistance patterns locally and nationally. This data informs treatment guidelines and identifies emerging threats early. Regulatory enforcement prevents over-the-counter antimicrobial sales and controls medicine quality.
Strategies to Combat Antimicrobial Resistance
Proven strategies to combat antimicrobial resistance exist and show effectiveness when implemented comprehensively. Antimicrobial stewardship programs in hospitals guide appropriate prescribing through protocols, education, and feedback.
- Pharmacists review antimicrobial orders, ensuring correct drugs at proper doses for adequate durations.
- Microbiology laboratories perform susceptibility testing, identifying which drugs will work against specific infections.
- Infection control committees monitor healthcare-associated infections and implement prevention measures.
- Public awareness campaigns educate communities about antimicrobial use and resistance risks.
- Educational programs train healthcare workers on prescribing guidelines and resistance mechanisms.
- Regulatory agencies enforce prescription requirements and prosecute illegal antimicrobial sales.
- Agricultural policies restrict antimicrobial use in food animals to therapeutic purposes only.
- Research programs develop new antimicrobials, rapid diagnostics, and alternative treatments.
Each strategy addresses different aspects of the resistance problem. Combined implementation creates a comprehensive defense against resistance development and spread.
Prevention Is Still Possible If Immediate Action is Taken
Antimicrobial resistance threatens to reverse decades of medical progress, but prevention remains achievable through coordinated action. Success requires commitment from government, healthcare systems, prescribers, pharmacies, agricultural sectors, and patients.
Prevention of antimicrobial resistance isn’t someone else’s responsibility. Every antibiotic prescribed, every infection prevented, and every treatment course completed affects the broader resistance landscape. The window for effective action is closing, but hasn’t shut.
Organizations working on antimicrobial stewardship coordination, education, and surveillance support efforts across Nigeria.
To learn more about evidence-based approaches and join national prevention initiatives, visit NNAST and contribute to protecting antimicrobial effectiveness for current and future generations.
FAQs
Can resistance be reversed once it develops?
Resistance is difficult to reverse completely, but can be reduced. When antimicrobial use decreases, resistant organisms lose their survival advantage, and susceptible strains may recover dominance. However, resistance genes often persist in bacterial populations. Prevention remains more effective than reversal.
What role do patients play in preventing resistance?
Patients significantly impact resistance through their behaviors. Using antimicrobials only when prescribed, completing full treatment courses, never sharing medicines, and practicing infection prevention all reduce resistance. Patient demand for unnecessary antimicrobials also drives inappropriate prescribing.
How effective are national policies in controlling resistance?
National policies work when enforced consistently. Countries with strict prescription requirements, antimicrobial stewardship mandates, and strong regulatory enforcement show slower resistance development. Policies without enforcement produce minimal impact. Nigeria’s challenge lies in implementation rather than policy existence.