In Nigeria, antibiotic resistance has become an unnoticed but significant public health concern in recent years. Once curable infections are now more difficult, sometimes impossible to cure, due to the growing abuse and overuse of antibiotics. In addition to putting lives in danger, this expanding crisis puts additional strain on Nigeria’s already overburdened healthcare system.
However, what does antibiotic resistance actually mean? How can it be handled before it gets out of control, and what causes it? This blog discusses the causes, consequences, and strategies needed to prevent the spread of drug-resistant bacteria in Nigeria.
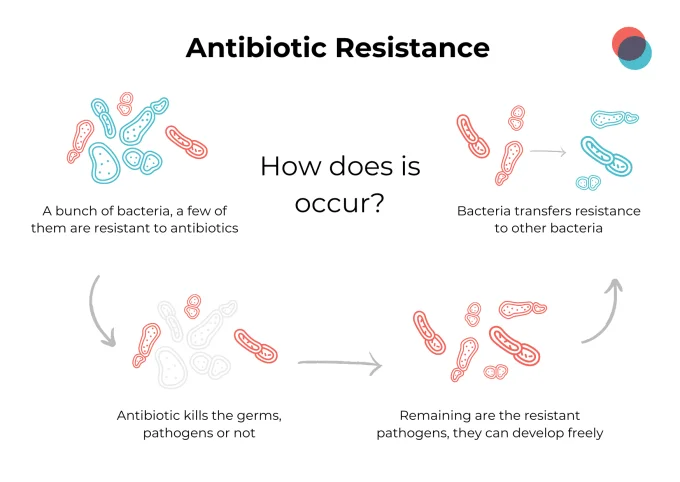
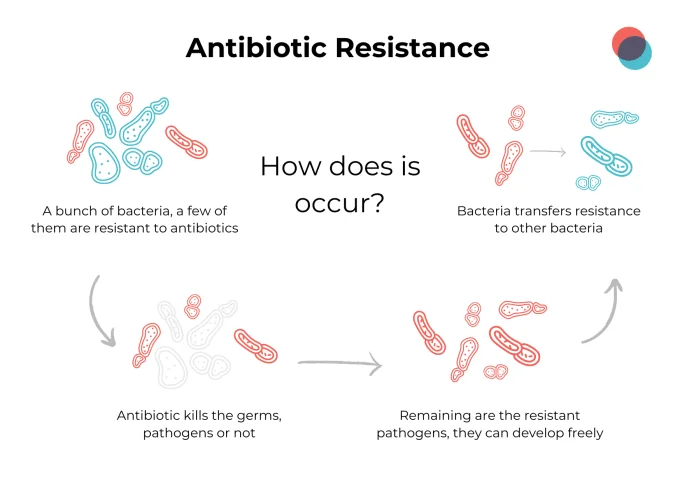
What Is Antibiotic Resistance?
Antibiotic resistance in simpler words means, when bacteria happens to evolve and develop the ability to break the drugs that are the most effective at killing them. This makes the standard medication ineffective causing the illness to get worse and might spread to other people.
The resistant bacteria that survives even when treated with strong medication are referred to as superbugs.
In developing nations like Nigeria, where public awareness is low, sanitation is poor, and government control is lax, this is much more of a worry.
The Current State of Antibiotic Resistance in Nigeria
Nigeria faces a distinctive and difficult battle with bacterial resistance. Studies provide the types of bacterial infections that have high resistance such as;
- Typhoid fever
- Urinary tract infections (UTIs)
- Tuberculosis (TB)
- Pneumonia
Thus, Nigeria is one of the nations with a high incidence of multidrug resistant TB and other bacterial illnesses, according to the World Health Organization (WHO).
Factors Contributing to Nigeria’s Crisis:
- Purchasing power of antibiotics over the counter without prescriptions
- Poor healthcare infrastructure
- Lack of diagnostic abilities
- Inadequate public awareness of how to prevent antibiotic resistance
This issue needs urgent measures, or else the country will be at high risk of entering a post antibiotic future, making even a minor injury life threatening.
Common Causes of Antibiotic Resistance
The first step in resolving the issue is to comprehend the underlying causes of resistance. The following are the main causes of antibiotic resistance in Nigeria:
1. Overuse and Misuse of Antibiotics.
Antibiotics are frequently used to treat viral infections such as the flu or common cold, both of which do not respond to antibiotics. With this sort of misuse, bacteria have never ending chances to adapt and evolve.
2. Self Medication and Over the Counter Purchase.
In many parts of Nigeria, antibiotics can be purchased over the counter or from a street pharmacist without a prescription. Many people will take the antibiotics incorrectly, incomplete dose or wrong antibiotic which can help speed up the process of resistance.
3. Agricultural Misuse.
Antibiotic use is widespread in livestock settings for purposes of growth promotion, disease prevention and treatment, whether the use is warranted or not. The incorrect use can cause animals to acquire resistant germs, which can then spread to people through the environment or food chains.
4. Poor Infection Control in Hospitals.
In some hospitals and particularly in more rural Nigeria, infection control precautions are not followed. There is poor sterilization, over crowded wards, reuse needles and uncontrolled sharing of antibiotic treatments. This also causes the spread of the superbugs.
Effects of Antibiotic Resistance
The consequences of antibiotic resistance are pervasive and alarming, particularly in low resource nations like Nigeria.
1. Increased Mortality Rates
More and more people die from infections that used to be curable. For example, neonatal sepsis is becoming less treatable due to antibiotic resistant strains of bacteria, as well as TB.
2. Prolonged Hospital Stays
Drug resistant infections take longer to treat, and many need new expensive drugs that are considered the last line of defense. This increases hospital stays and adds to the expenditures for already financially burdened households.
3. Economic Impact
Antibiotic resistance in Nigeria has a startling economic consequence. It reduces worker productivity, raises medical expenses, and takes funds away from other urgent public health requirements.
4. Danger to surgical and cancer patients
In order to prevent postoperative infections, many operations and cancer treatments depend on efficient antibiotics. Routine medical procedures become more dangerous as resistance increases.
Superbugs in Nigeria: A Growing Threat
Bacterial species known as “superbugs” are resistant to several antibiotics. The following superbugs are the most often reported in Nigeria:
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Multi-drug resistant Mycobacterium tuberculosis
- Extended-spectrum beta-lactamase (ESBL)-producing bacteria
Since patients are most at risk in newborn units, critical care units, and surgical wards, these pathogens are more harmful there.
Antibiotic Resistance Treatment Challenges
It is becoming harder and harder (and more expensive) to treat drug-resistant, and doctors often need to turn to toxic medications or combinations of multiple antibiotics which have a lot of side effects and don’t guarantee any positive outcome.
Challenges in Treatment:
- Restricted access to newer broader spectrum antibiotics
- Insufficient laboratory facilities for accurate diagnosis
- The limited presence of trained infectious disease specialists
- Counterfeit or substandard medications/xenobiotics
Healthcare professionals have limited resources to combat even common diseases in the absence of effective antibiotic resistance treatment.
How to Prevent Antibiotic Resistance: A Multi-Level Strategy
Combating antibiotic resistance in Nigeria calls for a collective, multi-sectoral commitment involving not only national government officials and health care providers, but also, farmers and the general public.
1. Regulating Antibiotic Sales
Government should implement strict policies and enforce national laws that prevent antibiotics from being sold over the counter and only licensed clinicians should prescribe the substances.
2. Public Awareness Campaigns
Informing the public about causes of antibiotic resistance including the correct ways to use antibiotics and the risks of self medication, would prevent much of the misuse.
3. Surveillance and Data Collection
The Nigerian Center for Disease Control (NCDC) and other related governmental authorities need to strengthen our national health data systems to track incidence of resistance, its trends and endemic outbreaks.
4. Improving Diagnostics
There are a number of fast and affordable diagnostic capabilities on the market that can provide rapid diagnostics to doctors for assessment of bacterial infections so they can consider antibiotics with caution and avoid unnecessary prescriptions.
5. Antibiotic Stewardship Programs
Hospitals should implement antibiotic stewardship programs that support the appropriate use of antibiotics, monitor resistance rates in their hospital and take actions based on their data; educate its staff on appropriate use and management of antibiotic resistance.
6. Infection Prevention in Healthcare
Routine hygiene practices, sterilization and waste disposal needs to be normal practices in hospitals and clinics to protect them from problematic superbugs that can cause outbreaks in their services.
7. Agricultural Controls
To minimize needless exposure to the larger environment, farmers should get training and regulations on how to properly utilize antibiotics in animals.
Global and Local Efforts in Combating Resistance
WHO’s Global Action Plan:
The World Health Organization’s Global Action Plan on Antimicrobial Resistance, which Nigeria has embraced, includes tactics like:
- Raising consciousness
- Increasing surveillance
- Lowering the frequencies of infection
- Making the best use of antibiotics
- Encouraging long-term research investment
Nigeria’s National Action Plan:
To address antibiotic resistance, the Federal Ministry of Health unveiled the National Action Plan (NAP). Implementation is still difficult, though, because
- Insufficient funds
- Poor stakeholder coordination
- Insufficiently skilled staff
- Low levels of public compliance
The Road Ahead: Turning the Tide
Antibiotic resistance in Nigeria can be stopped, but only with consistent work, financial support, and responsibility.
Important Steps to follow:
- Implement stronger rules for the distribution and usage of antibiotics.
- Boost financing for diagnostics, teaching, and research.
- To overcome challenges, unite the public health, veterinary, and agriculture sectors.
- Give them the information and resources they need to take antibiotics properly.
Conclusion
Antibiotic resistance poses a pressing yet treatable problem in Nigeria.
The problem is complex, yet the solutions are possible. All we need to do is to understand what antibiotic resistance is, be aware of the drivers, and encourage responsible behavior that will protect future generations from entering a world where antibiotics are no longer effective.
Now is the time for all of us whether you are a health professional, government policy maker, farmer or an ordinary citizen to act. When antibiotics lose their potency, we lose more than just medicine, we lose the fight for life itself.
FAQs
What is antibiotic resistance and why is it a problem?
When bacteria change and cease to react to antibiotics, antibiotic resistance results. Longer illnesses, greater fatalities, and more healthcare expenses result from this.
What are the main causes of antibiotic resistance in Nigeria?
The main reasons are overuse, self-medication, inadequate hospital infection control, and abuse in agriculture.
How can antibiotic resistance be prevented?
Using antibiotics just as directed, completing entire courses, maintaining better cleanliness, and controlling sales are all examples of prevention.
Are superbugs common in Nigeria?
Yes. Multidrug-resistant TB, ESBL-producing bacteria, and MRSA have all been documented in Nigeria, particularly in hospitals.
What is being done to fight antibiotic resistance in Nigeria?
Although complete implementation is still ongoing, Nigeria has created a National Action Plan and collaborates with WHO to enhance surveillance, increase awareness, and restrict the use of antibiotics.