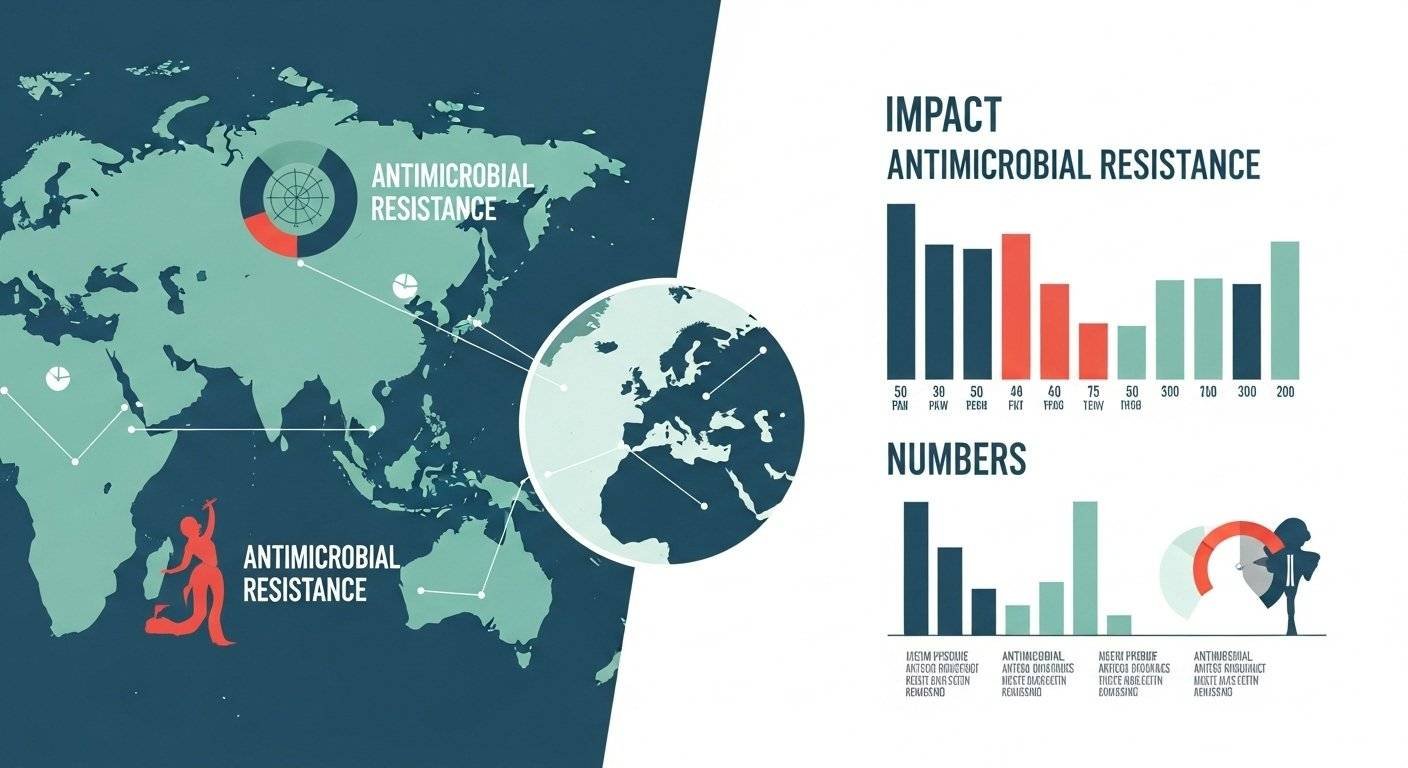
Antimicrobial stewardship in Nigeria’s resistance data reveals a disturbing reality that most health officials prefer not to discuss openly. The numbers exist but remain fragmented across hospitals, research institutions, and scattered surveillance sites.
Complete national statistics remain elusive, creating a knowledge vacuum where policy decisions drift without evidence. This data gap isn’t accidental. It reflects decades of underfunded surveillance systems, disconnected laboratory networks, and inadequate reporting infrastructure. Yet even incomplete data paints a concerning picture.
Multi-drug-resistant bacteria appear in Nigerian hospitals with increasing frequency. Treatment failures climb. Mortality from resistant infections rises.
Why Nigerian Resistance Data Demands Urgent Attention
The statistics of antimicrobial resistance in Nigeria affect healthcare delivery, economic productivity, and national security. When first-line antibiotics fail, patients require more expensive alternatives that strain both household budgets and healthcare systems.
Prolonged hospitalizations for resistant infections consume limited bed capacity, preventing admission of other patients needing care. Healthcare workers face increased occupational exposure risks when treating resistant infections. Agricultural productivity suffers when farmers lose income during extended illnesses.
Educational outcomes decline when children miss school due to recurring resistant infections. The mortality burden hits hardest in neonatal units and intensive care settings where resistant bacteria cause untreatable sepsis.
Each death represents not just personal tragedy but lost economic potential and community impact. Without accurate statistics, resource allocation remains guesswork. Interventions target assumptions rather than verified problems.
Policy makers lack justification for necessary investments in stewardship programs, laboratory infrastructure, and surveillance systems.
How AMR Surveillance in Nigeria Functions and Falls Short
AMR surveillance in Nigeria operates through scattered mechanisms that don’t connect into comprehensive networks. Academic medical centers conduct local surveillance for research purposes but rarely share data systematically. The Nigerian Antimicrobial Resistance Surveillance System attempts national coordination but faces challenges with laboratory capacity, reporting compliance, and data quality.
Many facilities lack basic microbiology laboratories capable of performing culture and susceptibility testing. Those with laboratories often struggle with supply shortages, equipment maintenance, and trained personnel retention.
Private laboratories generate data but operate independently without contributing to national surveillance. The pharmaceutical sector imports antimicrobials without systematic tracking of consumption patterns. Agricultural antimicrobial use remains completely unmeasured. Electronic health records that could facilitate automated resistance monitoring remain rare.
Manual reporting systems depend on overburdened healthcare workers who prioritize patient care over data entry. These gaps mean current statistics of antimicrobial resistance in Nigeria represent fragments rather than comprehensive pictures of the true resistance burden.
Evidence-Based Antibiotic Stewardship Depends on Reliable Data
Antibiotic stewardship programs require robust data for effective implementation. Stewardship interventions should target antimicrobials causing the most resistance problems locally. Formulary restrictions make sense only when data shows specific drugs driving resistance patterns. Prescriber education needs local examples demonstrating the consequences of inappropriate use.
Audit and feedback systems comparing prescriber patterns to evidence-based benchmarks require baseline data on current prescribing practices and resistance outcomes. Treatment guidelines must reflect local susceptibility patterns rather than generic recommendations.
Diagnostic stewardship promoting appropriate testing depends on understanding which infections require testing versus empirical treatment. De-escalation strategies moving patients from broad-spectrum to narrow-spectrum antimicrobials need susceptibility data confirming that narrower drugs will work.
Without data, antibiotic stewardship becomes theoretical recommendations disconnected from actual clinical conditions. With comprehensive statistics of antimicrobial resistance in Nigeria, stewardship becomes a precision intervention targeting verified problems with measurable outcomes.
Numbers Tell the Story We Can No Longer Ignore
The statistics of antimicrobial resistance in Nigeria remain incomplete but increasingly alarming. Available data demonstrates that resistance affects Nigerian patients now, not in some distant future scenario. AMR surveillance in Nigeria needs urgent strengthening to guide evidence-based responses.
Antibiotic stewardship interventions depend on reliable local data showing which resistance problems require the most immediate attention. Closing data gaps requires investment in laboratory infrastructure, reporting systems, and analytical capacity.
Policy decisions made without adequate statistics of antimicrobial resistance in Nigeria waste resources and miss opportunities for effective intervention.
At NNAST, we coordinate national surveillance efforts, strengthen laboratory capacity, and improve data systems to generate evidence that guides effective stewardship strategies.
FAQs
How reliable is AMR data in Nigeria currently?
Nigerian AMR data varies in reliability. Data from well-equipped research institutions using standardized methods is generally reliable. However, coverage remains limited geographically and by facility type. Many regions lack surveillance entirely. Equipment problems, supply shortages, and methodology variations affect data quality. National aggregated statistics should be interpreted cautiously.
Which pathogens show the highest resistance levels?
Staphylococcus aureus shows high methicillin resistance. Escherichia coli and Klebsiella pneumoniae frequently demonstrate extended-spectrum beta-lactamase production. Acinetobacter and Pseudomonas species show multidrug resistance in intensive care settings. Carbapenem-resistant Enterobacteriaceae appear increasingly, though they remain less common than in some other regions.
Why does surveillance matter for funding?
Funding agencies require evidence demonstrating need and impact. Without surveillance data, proposals cannot justify requested amounts or show baseline conditions against which progress gets measured. Good surveillance data strengthens funding applications, attracts donor interest, and demonstrates accountability through measurable outcomes tracking.