What Is antimicrobial resistance
What Is AMR?
What is AMR in simple words?
Antimicrobial Resistance (AMR) refers to a situation in which germs (microorganisms that cause infections) develop resistance to the medications used to treat them. These drugs used as treatment are called antimicrobials or antibiotics, and they kill or slow down microbial organisms. Bacteria, along with viruses, fungi, and parasites, comprise the microbial category. Over time, some of them change and fight back. This change makes medicines useless against those germs.
Some bacteria also acquire resistance tricks from other resistant bacteria. This gives them the ability to fight and become even stronger against more medicines. These tricks can make treatments slow or ineffective against infections that they used to be able to treat. It means treatments stop working like they should. Doctors then have to struggle to find other, sometimes more expensive and dangerous medicines that work, even as mild infections or those that were previously decreasing become more common and deadly again. Common infections and surgeries are risky when infections can’t be treated, and people may remain sick for longer periods. AMR leads to more testing, higher costs, and stress, people getting sicker, and unfortunately, some of these people die.
Understanding how these organisms and bacteria fight back and being able to identify, prevent, and treat them helps stop AMR.
AMR is not confined to one country, race, social class, or ethnic group. AMR extends across borders, affecting every country worldwide. That’s why AMR is a significant concern today.

How do bacteria and fungi become resistant to treatments
Germs change over time to survive drug attacks. These changes happen naturally through genetic shifts. Sometimes, one microbe shares its resistance with others. This makes the problem grow faster and broader. But natural change isn’t the only reason. Many human actions speed up this resistance.
Some common causes of antimicrobial resistance are:
- Taking antibiotics when they aren’t needed
- Not finishing the full dose or prescription
- Using antibiotics in animal feed or farming
- Poor hygiene in homes and health centers
- Dirty water and lack of clean toilets
What Makes Bacteria Resistant to Treatments
Antibiotic resistance mechanisms enable bacteria to survive medications that are prescribed to treat infections. Here are some ways bacteria resist treatment:
- They change their outer layer to block drugs
- They push the drug out of their cells
- They break down the drug using enzymes
- They hide in layers called biofilms

Global and National Action Plans
Many groups now treat AMR as a threat. The World Health Organization leads global AMR efforts. They set plans and support each country’s work. Nigeria has joined this fight as well. The country launched a national AMR plan in 2017. It focuses on research, education, and proper medicine use. Doctors, farmers, and health workers are all involved. There are still gaps in tracking resistance patterns. More training and better labs are also needed. But progress is happening step by step. Nigeria’s efforts will protect millions if done right. Strong leadership and funding can push it forward.
The Current Impact of Antimicrobial Resistance
Antimicrobial resistance is no longer a future risk. It’s already affecting lives, treatments, and health systems. Here's how AMR is changing daily life.

Infections Are Now Harder to Treat
The same medicines don’t always work anymore. People stay sick longer and face more problems.

Medical Procedures Are No Longer Safe
Surgeries and cancer care depend on antibiotics. Without them, even simple operations turn risky.

Some Diseases Are Coming Back Stronger
TB, bacterial infections that cause respiratory and urinary infections, simple cuts and wounds, and sexually transmitted diseases such as gonorrhea, are now more complicated to treat. Drug-resistant forms are harder to cure or stop.

Antibiotic Resistance in Nigeria
People often misuse antibiotics without testing. This misuse increases the spread of resistant infections.

AMR Hurts the Most Vulnerable
Babies, young children, pregnant women, and older adults face higher health risks. Weak immunity makes it harder to survive AMR.
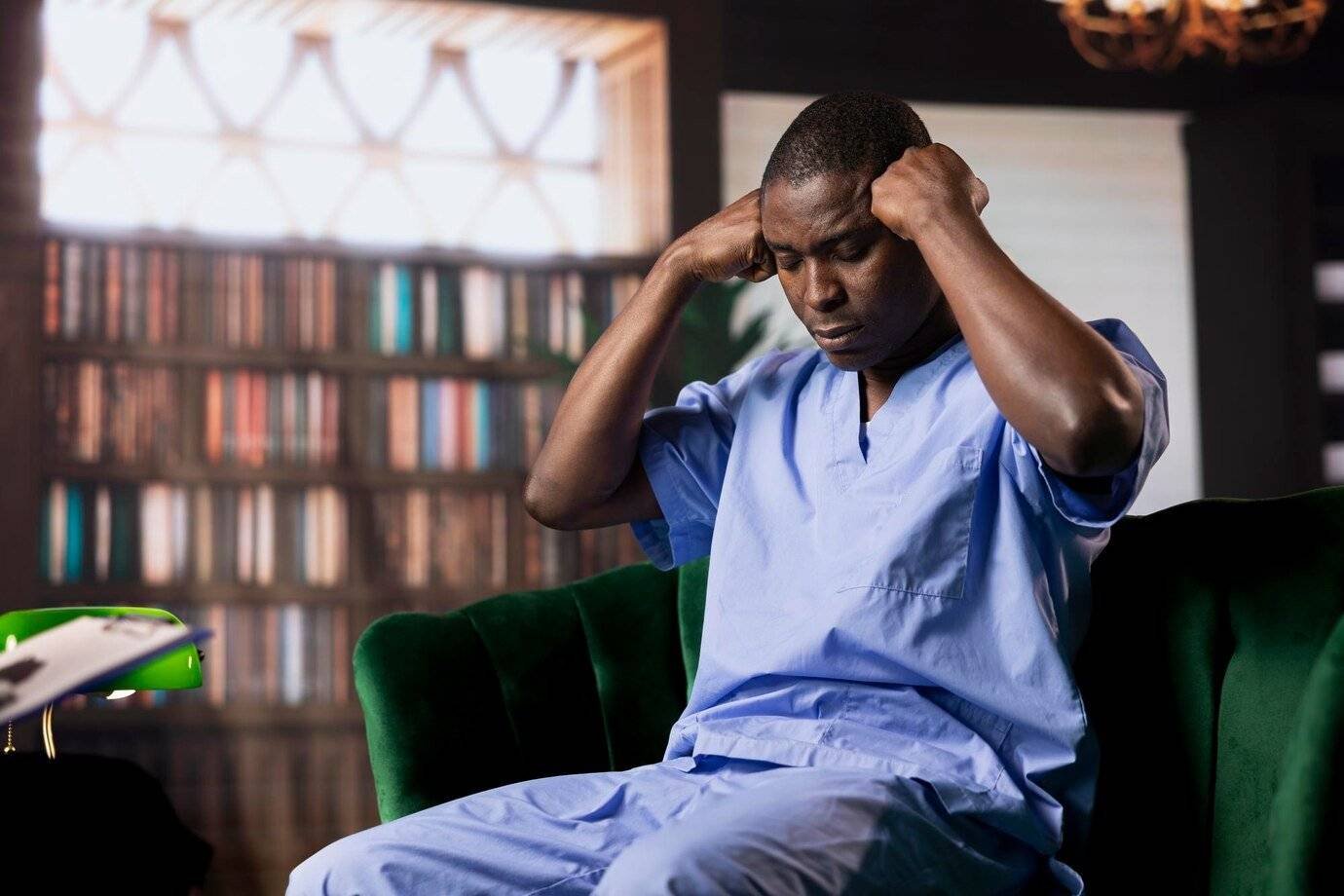
Hospitals Face Higher Costs and Stress
More time, more substantial and more expensive drugs, and more extended care are needed. AMR puts extra pressure on healthcare workers daily.
Some Diseases Are Coming Back Stronger
TB, bacterial infections that cause respiratory and urinary infections, simple cuts and wounds, and sexually transmitted diseases such as gonorrhea, are now more complicated to treat. Drug-resistant forms are harder to cure or stop.
EFFECTS OF AMR
The Current Impact of Antimicrobial Resistance
Antimicrobial resistance is no longer a future risk. It’s already affecting lives, treatments, and health systems. Here's how AMR is changing daily life.

Infections Are Now Harder to Treat
The same medicines don’t always work anymore. People stay sick longer and face more problems.

Medical Procedures Are No Longer Safe
Surgeries and cancer care depend on antibiotics. Without them, even simple operations turn risky.
Some Diseases Are Coming Back Stronger
TB, bacterial infections that cause respiratory and urinary infections, simple cuts and wounds, and sexually transmitted diseases such as gonorrhea, are now more complicated to treat. Drug-resistant forms are harder to cure or stop.

Antibiotic Resistance in Nigeria
People often misuse antibiotics without testing. This misuse increases the spread of resistant infections.

AMR Hurts the Most Vulnerable
Babies, young children, pregnant women, and older adults face higher health risks. Weak immunity makes it harder to survive AMR.
Hospitals Face Higher Costs and Stress
More time, more substantial and more expensive drugs, and more extended care are needed. AMR puts extra pressure on healthcare workers daily.

Solutions to Antimicrobial Resistance
There is no single fix for AMR. We need many actions at the same time. Everyone must take part, not just doctors. Here are some solutions to antimicrobial resistance:
Raising public awareness is also very important. People must learn when antibiotics help or not. Schools, media, and clinics must share this knowledge.
Antimicrobial research in Nigeria is now growing. Local experts are working on new treatments. They are also studying how germs resist drugs. This helps find better ways to stop AMR. But more funds and tools are still needed. Research takes time and strong team efforts.
Healthcare workers must check patients before administering medication. Using antibiotics for quick growth purposes should be avoided by farmers. Getting vaccinated reduces the occurrence of illnesses. Lower incidence of illness leads directly to lower antibiotic requirements.
- Only use antibiotics when they’re truly needed
- Get tested before starting any antibiotic treatment
- Never share or self-prescribe medicines
- Wash hands often and keep surroundings clean
- Don’t use antibiotics in animal feeds or farms
How to Prevent Antimicrobial Resistance
We can all help slow down this problem. Small actions make a big difference. How to prevent antimicrobial resistance? Start simple:
- Don’t pressure doctors to give antibiotics
- Finish every dose even if you feel fine
- Keep hands clean to stop infection spread
- Don’t use leftover drugs from past illnesses
- Make sure your food comes from safe sources

FAQs
AMR means germs no longer respond to medicines. It makes infections harder to treat and more dangerous. Everyone is at risk if AMR keeps growing.
Not fully, but it can be slowed down. Using antibiotics only when needed helps a lot. More research and better care can reduce the spread.
Only take antibiotics with a doctor’s advice. Keep good hygiene and finish your full treatment. Don’t share or buy antibiotics without reason.
Yes, it’s growing fast in Nigeria. People often use antibiotics without testing or guidance. This makes the spread of resistance much worse.


